The Steps to Longevity
Key Points:
- Chronic disease and deterioration of health don’t happen overnight. Poor nutrition, exercise, and a recovery program ensure long-term health.
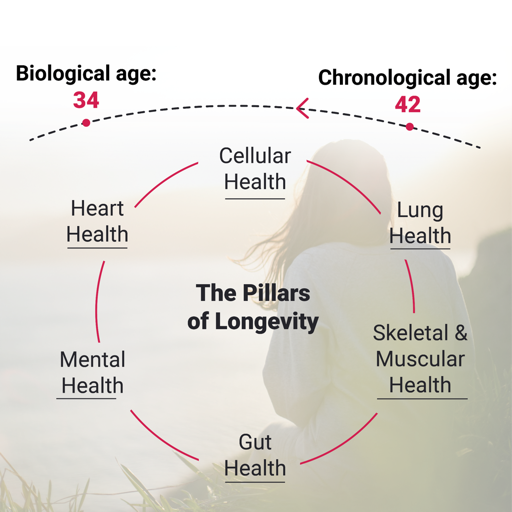
- Nutrition, training, and exercise all support the pillars of health and longevity, including Cellular, Heart, Lung, Gut, Mental, and Skeletal Muscle Health.
- Understand how each type of training, nutrition, and recovery elements impact each pillar of health and longevity.
Living a long, healthy life can be one of the most complicated goals. Most of us don’t know where to start, can’t establish a correlation between lifestyle choices and health benefits, and thus spend years experimenting based on empirical knowledge from health professionals, friends, and the media. It doesn’t have to be this way, though. Any significant and daunting endeavour can be turned into an achievable objective if you break it down into small, understandable, and actionable steps. This article discusses the pillars of longevity and the fundamental lifestyle choices influencing them. In simple terms, we aim to explain the focus areas and what you can do about them by leveraging nutrition, exercise, and recovery.
What is longevity made of?
Living a long and healthy life stems from ensuring that specific elements of our biology remain healthy. These include cardiovascular, pulmonary, cellular, skeletal muscle, mental, and gut health.
Heart health: Our cardiovascular system includes our heart, arteries, and veins and gives rise to the most common and costly chronic conditions, including heart failure, coronary artery disease, and hypertension. It’s the most common cause of death in the developed world; consequently, high cardiovascular health is a prerequisite for longevity.
Lung health: The American Lung Association elevated lung disease as the leading cause of death this year. Unlike popular belief, the degradation of lung health can be caused by several factors, including air pollution, infectious diseases (e.g., COVID-19), and chronic syndromes (e.g., COPD). Although pulmonary conditions may likely not be the immediate cause of death, their comorbidity with other more dangerous conditions, such as heart disease, threatens one’s life span. Moreover, their ability to hamper physical activity renders them a depreciation factor of life’s quality.
Cellular health: Cellular health is the third puzzle against chronic disease. Metabolic syndrome and obesity directly relate to how our cells utilize oxygen to burn nutrients and sustain life and power movement. Studies have now linked diabetes to our cells' inability to use oxygen effectively. Moreover, studies have shown that metabolic slowdown, where our cells use less oxygen and burn fewer calories than predicted, is the primary factor leading to weight loss failure. Obesity and diabetes consequently become the cause of life-threatening conditions such as heart disease and thus become the root cause of premature and, in most cases, expensive fatalities.
Skeletal & muscle health: Skeletal and muscle deficiencies such as lower back pain and hip displacement are the primary factors depreciating quality of life. Moreover, due to their debilitating effect on physical activity, they become the root cause of obesity and metabolic syndrome, leading to cardiovascular and pulmonary conditions. These will, in turn, lead to lower quality and span of life.
Mental health: Depression, stress, and anxiety can bring about physiological and life-threatening conditions through several pathways. First, they can be the root cause of physical activity and unhealthy eating habits. Moreover, as our blog post “The effects of chronic stress on energy balance” states, chronic stress can lead to several hormonal perturbations that promote visceral fat accumulation and increase the likelihood of metabolic syndrome independently of weight gain. The combination of these factors leads many to develop one or more common chronic conditions (i.e., cardiovascular, pulmonary, metabolic), leading to lower quality and span of life.
Gut health: Our gut is a complex “superorganism” that can positively or negatively affect our health in countless ways. An impaired gut microbiome can impair fat metabolism and energy absorption and affect our immune system, giving rise to a host of diseases, including pulmonary and metabolic syndrome. Moreover, our brain and gut are inextricably connected, which renders the gut microbiome a potent modulator of our mental health. Consequently, a healthy gut safeguards against metabolic, lung, cardiovascular, and cognitive disorders.
What can I do to live longer and better?
The short answer is to ensure all the systems mentioned above work correctly. To achieve this, however, one needs to employ different tools for each one of these systems. The table below summarizes the influence training, nutrition, supplementation, and recovery have on the other areas of our health.
Cellular health
Resistance training: Resistance training elevates your metabolism and prevents it from slowing down. This is of paramount importance as the metabolic slowdown is proven to be the most potent contributor to weight gain.
Interval training: Interval training increases growth hormone levels, essential for burning fat and maintaining and maintaining muscle mass.
Endurance training: Interval training increases growth hormone levels, essential for burning fat and maintaining muscle mass.
Micronutrient balance: Micronutrients have a central role in human metabolism. They are required for the appropriate functioning of energy production in the cells by metabolizing carbohydrates, proteins, and fats. A shortfall in any of them will be rate-limiting for energy production, with potential metabolic complications.
Macronutrient balance: Macronutrients are the nutritional components of food that the human body needs in large amounts for energy production (metabolism) and maintaining physiological functions. They include carbohydrates, fat, and protein. The diet macronutrient ratio doesn't directly influence weight. To optimally manage your weight, find a ratio you can stick with, whether a low-fat diet or a low-carb diet, etc., focus on healthy food choices across all food groups, and eat fewer calories than you burn.
Energy balance: Energy balance is the state achieved when energy intake from food equals energy expenditure from everyday activities and calories burnt at rest to perform essential functions such as breathing, heart beating, etc. (RMR). When the human body is in energy balance, body weight is stable. Body weight will decrease when the energy intake is lower than the energy expenditure, otherwise known as a caloric deficit. Irrespective of the type of diet (keto, vegetarian, Mediterranean, etc.) through which this caloric deficit will be accomplished, the most essential weight loss driver is the caloric deficit per se. With a sufficient caloric deficit, weight loss will be feasible. Body weight will increase when the energy intake is higher than the energy expenditure, otherwise known as caloric surplus.
Meal-timing: Meal timing may be crucial in obesity and weight loss treatment. In particular, it may affect 24-hour body cycles (circadian rhythm) that can predict weight loss. For example, night shift workers have an increased risk for obesity and may experience an increased appetite for energy-dense foods. More specifically, for people with the highest caloric intake until 2 hours before bedtime, the so-called evening chronotypes, the probability of being obese increases five times compared to people who eat the most significant proportion of their daily calories two hours after waketime, the so-called morning chronotypes. Moreover, it has been shown that eating your lunch late (after 3 p.m.) predicts difficulty in weight loss. However, meal timing can only be a potential tool to combat obesity since a sufficient caloric deficit will always be the most crucial determinant.
Adequate sleep: Maintaining a consistent sleep schedule with sufficient sleep time is vital for maintaining normal hormonal function, regulating hunger, and preventing stressed eating. It's also critical for recovering effectively and thus maintaining muscle mass and high metabolism.
Mental Health
Resistance/Interval/Endurance training: Every form of physical exercise significantly reduces stress, depression, and anxiety.
Micronutrient balance: Inadequate intake of micronutrients, which are particularly important for mental health, has been associated with inflammation in the central and peripheral nervous system (neuroinflammation); hence, mental disorders such as depression, sleep disorders, stress, and anxiety. Vitamin E, B12, folate, and magnesium are the most important micronutrients for mental health.
Macronutrient balance: A healthy dietary pattern affects not only the brain composition, structure, and function but also hormones, neuropeptides, and neurotransmitters, which play a crucial role in mental health. Fat is the most essential macronutrient for mental health, especially the omega-3 polyunsaturated fatty acids EPA and DHA. They are found primarily in fatty fish, such as salmon, sardines, and fish oil. They can help alleviate mood disorders such as depression symptoms and decrease antidepressant medication dosages.
Energy balance: Obesity is positively associated with various mental health issues, including depression, anxiety, and eating disorders. Obesity also impacts the quality of life, with many obese people experiencing increased stigma and discrimination because of their weight.
Meal timing: Irregular meal timing has been associated with higher productivity loss through more significant problems with sleep and stress. It has also been correlated with higher neuroticism and lower subjective overall well-being scores and perceived mental health.
Adequate sleep: Maintaining a healthy schedule is critical for regulating anxiety and mental health. Sleep and mental health are undeniably connected bi-directionally, with sleep deprivation or sleep schedule distortion being fundamental drivers of all mental health issues ranging from anxiety to depression and panic attacks.
Muscle and Skeletal Health
Resistance/Interval/Endurance training: Resistance training is critical for maintaining bone density, joint strength, and proper posture. High bone density is essential for averting osteoporosis with aging, whereas joint strength and correct posture are essential for avoiding common injuries like lower back pain.
Micronutrient balance: Inadequate intake of micronutrients that contribute to the antioxidative capacity of the cells, such as vitamins A, B6, B12, and E, folate, selenium, and zinc, may be related to increased muscle fatigue and frailty. On the other hand, the micronutrients of most significant importance for bone health and, hence, osteoporosis prevention are calcium and vitamin D.
Macronutrient balance: An increased dietary protein intake is recommended to prevent bone loss. A higher percentage of carbohydrate energy intake is associated with a higher risk of low bone mineral density. Therefore, the isocaloric substitution between carbohydrates and protein is significantly associated with bone health. Similarly, protein is the essential macronutrient for gaining and maintaining muscle strength and size. However, all three macronutrients through a healthy, balanced diet are crucial to developing and maintaining muscle mass.
Energy balance: Increased body fat typically accompanies a concomitant increase in fat deposition within skeletal muscle, leading to sarcopenia (progressive loss of muscle mass and strength) and physical disability. The increase in fat mass is also frequently associated with a simultaneous decrease in muscle mass and, therefore, a reduced metabolic rate. Hence, sarcopenic obese individuals burn fewer calories at rest, and their progressive muscle weakness leads them to chronic inactivity and, thus, even lower energy expenditure. On the other hand, obesity may increase bone density because it is associated with higher mechanical loads, which may protect bones. However, overly obese people (BMI>35) are more likely to fall and break bones; hence, over a certain BMI, obesity does not protect against fractures and may even increase their risk.
Meal timing: Although meal timing does not somehow affect muscle and skeletal health, nutrient timing, i.e., when relative to exercise, someone ingests their macronutrients, carbohydrates, and protein, in particular, seems to maximize the muscle stimuli of the exercise that has been preceded. Protein is vital to supporting muscle growth and muscle recovery. Consuming 20g of protein within 30 minutes to 2 hours after exercise, particularly resistance training, will help the muscle tissue recover and aid skeletal muscle growth. This amount of protein is recommended to be complemented by a sufficient amount of carbohydrates in a ratio of 1:3 or 1:4.
Adequate sleep: A healthy sleep schedule is equivalent to adequate physical recovery. Too short or too long a sleeping schedule has been linked to skeletal muscle problems like lower back pain.
Gut Health
Resistance/Interval/Endurance training: All forms of exercise have been shown to elicit positive effects on the gut microbiome. Specifically, exercise:
- Reduces intestinal permeability (the degree to which the surface of the digestive system is permeable to substances), thus blocking pathogens that may be found in the gut from entering the bloodstream.
- Increases the diversity of beneficial gut bacteria that aid digestion.
Micronutrient balance: Micronutrients can modulate the diversity and composition of the gut microbiome, leading to the prevalence of beneficial bacteria and gut health or harmful bacteria and gut and overall health complications. This relationship is bidirectional since gut bacteria synthesize essential micronutrients, considerably impacting the micronutrient balance.
Macronutrient balance: Macronutrients have various effects on gut health, both positive and negative. Specifically, non-digestible plant-derived carbohydrates, named dietary fibre, can improve gut microbial diversity and promote gut health. Dietary fibre increases the population of health-beneficial bacteria, such as Bifidobacterium and Lactobacillus. On the other hand, diets rich in saturated fat mainly derived from full-fat dairy products and animal-based foods such as beef and lamb harm the richness and diversity of gut microbiota.
Energy balance: The microorganisms that live in our gut (gut microbiota) could play a significant role in whether or not we become obese. Also, obesity per se seems to be able to change the composition of our gut microbiota by reducing its diversity and favouring a higher proportion of gut Firmicutes species compared to the Bacteroidetes species. These changes are associated with more marked overall fat accumulation and metabolic complications such as increased blood lipids (cholesterol) and glucose. Therefore, obesity and gut health share a bi-directional relationship where one determines the state of the other.
Meal timing: Meal timing does not seem to affect gut health in any other way other than increasing the possibility of experiencing heartburn and gut distress symptoms such as abdominal pain, bloating, etc., in general when having your large meal close to bedtime.
Adequate sleep: A healthy sleep schedule is critical for maintaining a healthy gut. Low sleep efficiency, sleep disturbances, and irregular sleeping windows have been proven to negatively affect the gut microbiome in several ways. A compromised gut microbiome leads to digestive, metabolic, and mental disorders.
Heart Health
Resistance/Interval/Endurance training: Interval and endurance training are heart health's most potent positive factors. They positively affect all areas of the cardiovascular system, including the heart and blood, arteries, and veins. Specifically, they:
- Strengthen the heart muscle
- Prevent arterial clogging
- Improve hemoglobin content in the blood
Micronutrient balance: A diet that prioritizes the consumption of a range of heart-healthy nutrients, including magnesium, potassium, B vitamins, vitamin D, and selenium, through the consumption of a variety of fruits and vegetables at every meal can lower the risk of coronary heart disease, stroke, and the overall incidence of cardiovascular diseases.
Macronutrient balance: Macronutrient balance has been linked to cardiovascular disease and related risk factors (high LDL and low HDL cholesterol). Specifically, increasing the consumption of monounsaturated fat (olive oil), omega-3 polyunsaturated fatty acids (fatty fish), and good-quality carbohydrates (whole grains, fruits, vegetables) while decreasing the amount of saturated fat (full-fat dairy products, animal-based foods) and refined grains (sweets, white carbs) can reduce the risk of cardiovascular disease.
Energy balance: Obesity accelerates the risk of developing cardiovascular disease by increasing circulating lipids (blood cholesterol and triglycerides) and blood pressure. Obesity is also associated with chronic inflammation and progressive physical activity decline and thus cardiorespiratory fitness, compromising heart health even more. This association is powerful when the excess fat deposition is in the abdominal area. This fat is called visceral fat and accumulates around vital organs, progressively leading to heart health issues.
Meal timing: Nighttime eating, defined as consuming food after bed, has been associated with a 55% greater risk of cardiovascular disease than non-nighttime eating. Although eating your largest meal late in the day could pose a greater risk for heart health issues, most results arise from observational studies and not from clinical studies, which would address the causality between meal timing and cardiovascular disease. Such studies have failed to demonstrate a direct link between meal timing and heart health. Therefore, based on current scientific evidence, meal timing is not a strong determinant of heart health.
Adequate sleep: A healthy sleep schedule is essential for preserving cardiovascular health. During sleep, blood pressure is reduced, and consequently, lack of sleep inevitably means that your blood pressure will remain higher for longer during the day. Elevated blood pressure is the most prominent risk factor for developing life-threatening heart conditions.
Lung Health
Interval/Endurance training: Interval and endurance training are the most potent positive factors of lung health. They positively affect all areas of the respiratory system, including the lungs and respiratory muscles. Specifically, they:
- Strengthen the respiratory muscles
- Improve oxygen transfer efficiency in the alveoli
- Increase vital lung capacity
Micronutrient balance: Certain micronutrients have anti-inflammatory and anti-oxidative properties, which can directly target the pathogenesis of lung function decline, such as chronic obstructive pulmonary disease, and thus promote lung health. These are vitamin A, vitamin E, vitamin C, and selenium.
Macronutrient balance: Carbohydrate metabolism acutely increases CO2 production and may deteriorate lung function in the long term, especially in older adults. Indeed, a carbohydrate-rich diet has been negatively associated with health markers of lung function, such as the FEV1, whereas protein and fat intake are inversely associated with lung function decline. This relationship is more powerful when carbohydrates derive from food sources rich in refined carbohydrates (sweets, refined grains) with low dietary fibre content.
Energy balance: Obesity is a significant risk factor for asthma, obstructive sleep apnea, and obstructive pulmonary disease. It also increases susceptibility to respiratory infections, and hospitalization rates are higher in obese patients with respiratory disease than in healthy-weight individuals. Fat accumulation in the abdominal area (visceral fat) is especially linked to asthma and impaired lung function, changing the normal physiology and part of the lungs.
Adequate sleep: Sleep deprivation has been shown to elicit the loss of breathing control, a risk factor for developing respiratory disorders such as asthma and COPD.
An Ounce of Prevention - Hyperion Health Blog